If you've ever struggled with persistent redness, bumps, or breakouts on your face, you may have wondered: Is it acne, rosacea, or both? These two common skin conditions can look remarkably similar, especially in their papule and pustule forms, but they have different causes, triggers, and treatments. Misdiagnosis can lead to ineffective or even aggravating skincare routines.
In this comprehensive guide, we'll break down the key differences between rosacea and acne, from symptoms and triggers to treatment strategies and prevention tips.
Understanding Rosacea and Acne
What is Rosacea?
Rosacea is a chronic skin condition that primarily affects the central face, causing redness, visible blood vessels, and sometimes acne-like bumps. It's more common in individuals aged 30 to 50 and can be triggered by various environmental and lifestyle factors.
What is Acne?
Acne vulgaris is a skin condition that occurs when hair follicles become clogged with oil and dead skin cells, leading to blackheads, whiteheads, and pimples. It's most common during adolescence but can affect individuals of all ages.
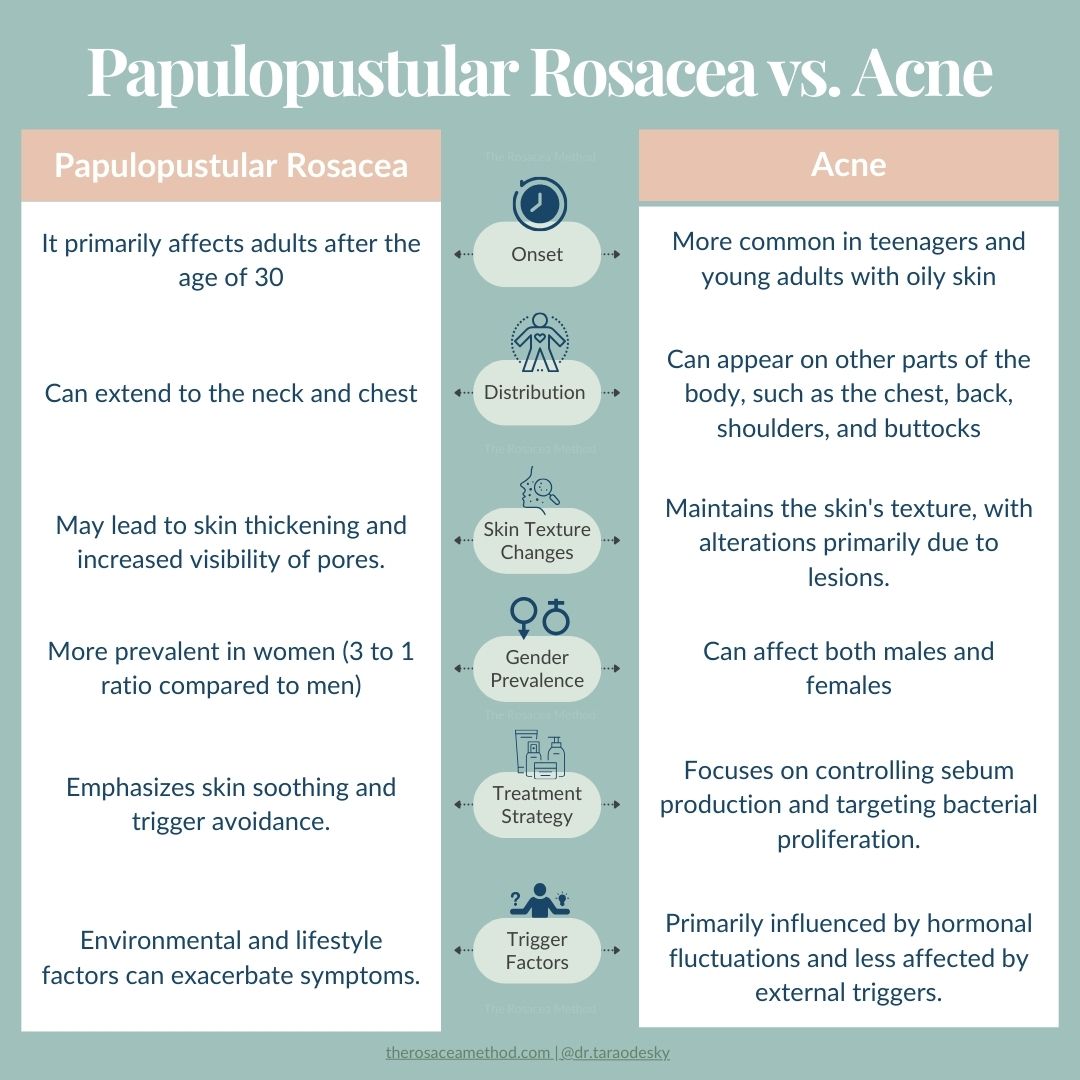
Key Differences Between Rosacea and Acne
Symptoms and Signs
Rosacea Symptoms
- Persistent facial redness
- Visible blood vessels (telangiectasia)
- Swollen red bumps resembling acne
- Burning or stinging sensation
- Eye irritation (ocular rosacea)
Acne Symptoms
- Blackheads and whiteheads
- Papules and pustules
- Nodules and cysts in severe cases
- Oily skin
- Potential scarring
Common Triggers
Rosacea Triggers
- Hot drinks and spicy foods
- Alcohol consumption
- Sun exposure
- Stress and strong emotions
- Extreme temperatures
Acne Triggers
- Hormonal fluctuations
- Certain medications
- Diet high in refined sugars
- Stress
- Use of oily or comedogenic skincare products
Diagnosis and Misdiagnosis
Differentiating between rosacea and acne can be challenging due to overlapping symptoms. However, the presence of comedones (blackheads and whiteheads) is a hallmark of acne, while rosacea is characterized by persistent redness and visible blood vessels without comedones.
Misdiagnosis can lead to inappropriate treatments. For instance, using acne medications on rosacea can exacerbate the condition. Therefore, consulting a dermatologist for an accurate diagnosis is crucial.
Treatment Options
Rosacea Treatments
- Topical antibiotics (e.g., metronidazole)
- Oral antibiotics for severe cases
- Laser therapy for visible blood vessels
- Avoidance of known triggers
Acne Treatments
- Topical retinoids
- Benzoyl peroxide
- Oral antibiotics
- Hormonal treatments (e.g., birth control pills)
- Isotretinoin for severe cases
Skincare Tips
- Use gentle, non-comedogenic cleansers
- Apply broad-spectrum sunscreen daily
- Avoid harsh exfoliants and alcohol-based products
- Moisturize regularly to maintain skin barrier
- Patch test new products before full application
When to See a Dermatologist
- Persistent or worsening symptoms
- Uncertainty about the condition
- Ineffectiveness of over-the-counter treatments
- Development of scarring or skin thickening
FAQs
Q: Can I have both rosacea and acne simultaneously?
A: Yes, it's possible to have both conditions at the same time, which can complicate diagnosis and treatment.
Q: Is rosacea contagious?
A: No, rosacea is not contagious.
Q: Can diet affect rosacea and acne?
A: Yes, certain foods can trigger rosacea flare-ups, and high-glycemic diets may exacerbate acne.
Q: Are there any permanent cures for rosacea or acne?
A: While there is no permanent cure, both conditions can be effectively managed with appropriate treatments.
Q: Does sun exposure worsen rosacea?
A: Yes, sun exposure is a common trigger for rosacea flare-ups.
Conclusion
Understanding the differences between rosacea and acne is essential for effective treatment and management.
While they may appear similar, their causes, triggers, and treatments differ significantly. Consulting a dermatologist for an accurate diagnosis ensures that you receive the most appropriate care for your skin condition.
Note: This article is intended for informational purposes only and does not substitute professional medical advice. Always consult with a healthcare provider for medical concerns.
